Trans Urethral Resection of Bladder Tumor (TURBT) in India starts from $2900. The total cost of the treatment depends on the diagnosis and facilities opted by the patient.
Cancer in Bladder can be found to vary depending on the type of its origins. It can arise from the lining of the epithelium which is the inner lining of the urinary bladder or the urothelium. Rare forms of cancer are not of epithelial origins like the sarcoma or lymphoma. Tumours in bladder is found to be the 9th leading type of cancer in United States as per a survey conducted in 2012 with 430,000 new cases and mortality of 165000 deaths annually.
About Trans Urethral Resection of Bladder Tumor
The first and foremost question to ask is where is your bladder located? The sac like muscular urinary bladder is located in the pelvis region above the pelvic bone. It is connected to the kidneys through the two ureters that transfer the urine from the kidney to the bladder for storage. An abnormal growth of cells in the inner lining causes a tumour requiring diagnosis and then followed by a turbt surgery.
In most cases the tumour cannot be assessed in the primary stages. There are hardly any notable evidences found when the patient is harbouring a primary tumour.
The next stage is designated as Oa and categorized as a non invasive type papillary cancer.
In the stage next of the stage 0 or the carcinoma in situ the inner lining of the bladder is affected and is still considered non invasive.
In stage I the cancer has spread into the lining of the bladder further but has not affected the muscular wall of the bladder.
While in Stage II the inside part gets affected including the muscles of the bladder making it now invasive.
And when the cancer has spread enough in muscles and the tissues around the bladder like the reproductive organs it is considered to be in stage III.
And in the final or stage IV the cancer will spread to the lymph nodes affecting the organs around it as well.
Causes of developing a tumour in bladder
The causes of tumour in bladder are not always very clear and well defined but it has been linked with smoking, chemical exposure and radiation or a parasitic infection. The abnormal cells undergo some mutation that allows them to multiply in a non orderly fashion and goes beyond control and they do not die thus giving rise to the tumour.
Symptoms of the TURBT
A person suffering from a tumour will experience mild sensation of burning and discomfort in the times of urination for quite a few days. The force of the urinary stream may also undergo significant changes which can be observed for a week to a fortnight. Usually there could be none of the symptoms and in certain cases all symptoms even if experienced may not lead to the conclusion that it is a bladder cancer. There can be blood or clots of blood in the urine along with a tendency of urinating too frequently. Tendency of urinating at night may be felt more but there can be general problems in urine passing. Associated along with this the patient can experience pain on either side of the body.
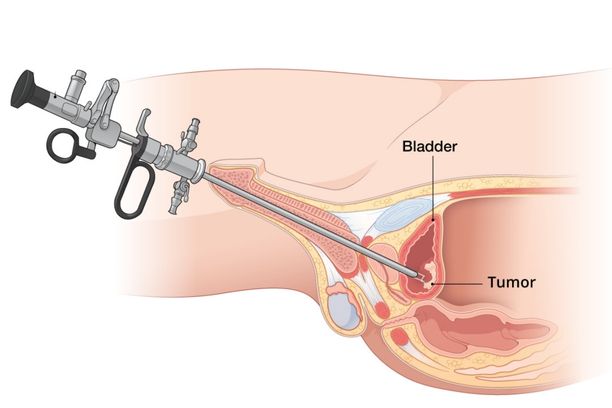
What is transurethral resection of bladder tumour?
This procedure aims at removing bladder tumours at an early stage by inserting a scope through the urethra leading to the bladder. In the TURBT procedure bladder cancer can be detected by the urologist and potentially allow the urologist to treat various other kinds of bladder related disorders. But 75% of the cancer of bladders that are detected are superficial in nature causing growth only on the surface of the walls of the bladder and does not get very deep. So this facilitates the surgeon to have the tumour removed at the bladder wall level causing no damage to the deeper layers of the organ. The information that is collected while executing the procedure will help the surgeons to decide the type of the abnormality of the tumour and the extent of the tumour. This later allows the urologist surgeons to decide whether further treatments will be required or not.
What are the alternatives for TURBT procedure?
Some of the other treatment alternatives for TURBT are being worked upon while some of them have tremendous side effects
Blue light fluorescent cystoscopy : Enhanced tumour visualization is possible and detection of tumour chances are increased by almost 20 to 25% with this method where an ultraviolet blue light is used. A dye is injected an hour prior to the procedure.
Adjuvant bladder cancer therapy: TURBT is not suitable for many who have high chances of suffering a recurrence within 12 months from the treatment. In this case adjuvant therapy is recommended. It includes intravesicle chemotherapy. Chemotherapy for bladder cancer includes giving medication to curb the abnormal growth of cells. But it also has its sets of side effects like experiencing irritation in bladder and loss of hair, nails and feeling debilitated for a very long period of time.